
Chronic pain sufferers should take exercise, not analgesics/medication/prescribed drugs says NICE.
Medicines watchdog recommends physical and psychological therapies when treating pain with no known cause.
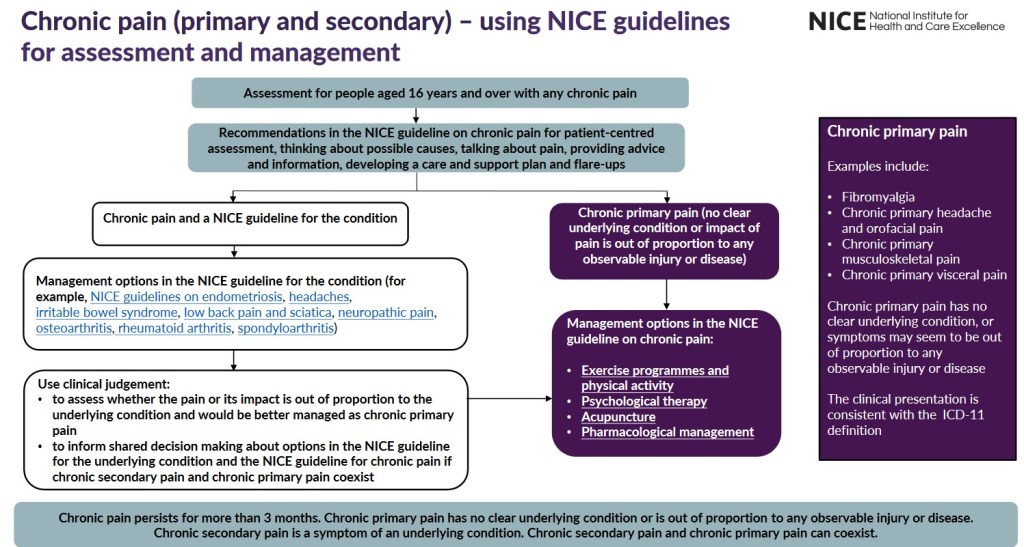
People suffering from chronic primary pain which is labelled as having, no known cause, should not be prescribed painkillers, the medicines watchdog has announced, recommending such patients be offered exercise, talking therapies and acupuncture instead.
In a major change of pain treatment policy, the National Institute for Health and Care Excellence (NICE) say that in future, doctors should advise sufferers to use physical and psychological therapies rather than analgesics to manage their pain. Medical teams can also consider prescribing antidepressants, the government health advisers suggest.
NICE’s new guidance potentially affects the way many hundreds of thousands of people in England and Wales tackle their condition because between 1% and 6% of the population of these nations is estimated to have chronic primary pain.
According to NICE, there is “little or no evidence” that treating the condition with painkillers makes any difference to the person’s quality of life, or the pain they suffer or their psychological distress, according to its new guidelines on the assessment and management of chronic pain.
Pain caused by a known underlying health condition such as osteoarthritis, rheumatoid, arthritis, ulcerative colitis or endometriosis is known as chronic secondary pain. However, pain with no identified cause that has persisted for at least three months is known as chronic primary pain.
Nice recommends that doctors draw up a care and support plan with patients about how to manage their pain based on how badly it is affecting their day-to-day life, what activities they feel they can undertake and honesty “about the uncertainty of the prognosis”.
The plan should include “interventions that have been shown to be effective in managing chronic primary pain. These include exercise programmes and the psychological treatments cognitive behavioural therapy (CBT) and acceptance and commitment therapy (ACT).
“Acupuncture is also recommended as an option, provided it is delivered within certain clearly defined parameters,” NICE says.
The antidepressants amitriptyline, citalopram, duloxetine, fluoxetine, paroxetine or sertraline can also be used, it adds.
Sufferers should not be started on commonly used medications such as paracetamol, non-steroidal anti-inflammatory drugs, benzodiazepines or opioids, which poses risks including addiction, the watchdog says. Dr Paul Chrisp, director of NICE’s centre for guidelines, said: “Based on the evidence, for most people it’s unlikely that any drug treatments for chronic primary pain, other than antidepressants, provide an adequate balance between any benefits they might provide and the risks associated with them.”
The Royal College of GPs backed the shift away from painkillers but cautioned that patients’ access to the new forms of treatment being recommended was variable.
Prof Martin Marshall, the college’s chair, said: “Pain can cause untold misery for patients and their families. Chronic primary pain… can be challenging to manage in general practice, and the college has been calling for guidelines to address this for some time.
“We understand the move away from a pharmacological option to treating chronic primary pain to a focus on physical and psychological therapies that we know can benefit people in pain.
“However, access to these therapies can be patchy at a community level across the country, so this needs to be addressed urgently, if these new guidelines are to make a genuine difference to the lives of our patients with primary chronic pain.”
Lucy Ryan, a patient representative who helped Nice draw up the new guidelines, welcomed its acknowledgement of the risks that a regime of tablets for chronic primary pain can involve because patients are sometimes not told about those.
“Everyone with chronic pain experiences pain differently, so I feel the more options available to help people effectively manage their pain, the better,” she added.
Source-https://www.theguardian.com (7th April 2021) Digital edition
******************************************************************
When I first read the above article in the Guardian newspaper, I was taken aback when other newspapers reported on the same information, but with different interpretations of what is being said. One such paper, claimed that NICE has said that anyone with chronic pain would be taken off prescribed painkillers!
This is not what is being said. If I copy and paste a paragraph here, there are two variations: one of chronic secondary pain and two of chronic primary pain.
Pain caused by a known underlying health condition such as osteoarthritis, rheumatoid, arthritis, ulcerative colitis or endometriosis is known as chronic secondary pain. However, pain with no identified cause that has persisted for at least three months is known as chronic primary pain.
Is this a money saving exercise by the Health Boards? Many people have chronic pain, and for years their health care providers have been unable to label or diagnose what the cause of the pain is. Individuals with chronic pain are therefore categorized into a group for chronic primary pain. What about the individuals that have unexplained pain, which science cannot pin-point? This pathway advises sufferers to come off painkillers and start exercise and receive acupuncture, hypnotherapy, talking therapies or other psychotherapy programs like MBCT. It is all very black and white to the reader, and will cause a lot of pain and upheaval for some, and a blessing for others.
Feel free to comment on your experience/thoughts on the above.
Thanks for reading
Steve

Interesting and relevant topic! I know there are people who can take benzodiazepines or opioids occasionally without problems, but in my 30 years as a substance abuse counselor, I saw many people who had great difficulty stopping these drugs. Tolerance – needing more to get the same effect – was also a problem. In the US it’s very hard to get alternative therapies covered by insurance. I’ve benefitted from acupuncture and massage therapy but have to pay “out of pocket” so don’t go that often. Carefully planned, gentle exercise can help most people. Swimming is a good example. It would be great if people got assistance paying for personal exercise trainers and alternative therapies.
LikeLiked by 4 people
Thank you for your input JoAnna, very helpful and supportive.
LikeLiked by 1 person
Without judging anyone, I find it unfortunate that such a fundamental principle of life needs to be told to people.
LikeLiked by 1 person
It has been so uplifting of late (the past couple of years in particular). I am becoming aware of many general practitioners taking it upon themselves to learn more about natural therapies, diet and exercise, etc., in regard their patient’s health. So long in coming. However, it has begun and can only increase over time.
LikeLiked by 1 person
I react to medications, so it is best for me to seek alternative medications. After getting an infection for osteopenia, I’m in the middle of a full fibromyalgia flare up but other pains I’ve never had before. I wish I hadn’t had it.
LikeLiked by 2 people
Hi Mary and thank you for your experience relating to medications. Fibromyalgia is unimaginable pain to many, and I hope that you feel less and more comfortable soon. Take care
LikeLike